Learn with VANA: How Does Opting-Out Work?
It’s critical to remember that opt-out does not change scope of practice laws for CRNAs, it only impacts reimbursement policy with the Centers for Medicare & Medicaid Services.
Opt-out specifically addresses Part A of the Centers for Medicare & Medicaid Services (CMS) requirements, known as the Conditions for Participation (CoP), for hospitals and facilities to be reimbursed by Medicare and Medicaid for anesthesia services that are provided by a CRNA. It does NOT have any bearing on Part B which addresses reimbursement for actual services rendered by a CRNA provider.
The federal requirement for CoP has been that CRNAs must be supervised by a physician, any physician not necessarily a physician anesthesiologist, in order for the hospital or facility to be reimbursed by CMS. The November 13, 2001 rule allows states to “opt-out” or be “exempted” (the terms are used synonymously in the November 13 rule) from the federal supervision requirement.
Thus, in opt-out states, hospitals and facilities that provide healthcare and anesthesia services provided by a CRNA are qualified to collect funds from CMS for those services without meeting the physician supervision requirements or guidelines. In short, this allows for many facilities across the country, especially in rural areas, to collect much needed revenues for those services without the unnecessary oversight. Since the rule was implemented in 2001, 25 states and Guam have either fully or partially opted out of the requirement successfully.
For a state to “opt-out” of the federal supervision requirement, the state’s governor must send a letter of attestation to CMS. The letter must attest that:
- The state’s governor has consulted with the state’s boards of medicine and nursing about issues related to access to and the quality of anesthesia services in the state; and
- That it is in the best interests of the state’s citizens to opt-out of the current federal physician supervision requirement; and
- That the opt-out is consistent with state law.
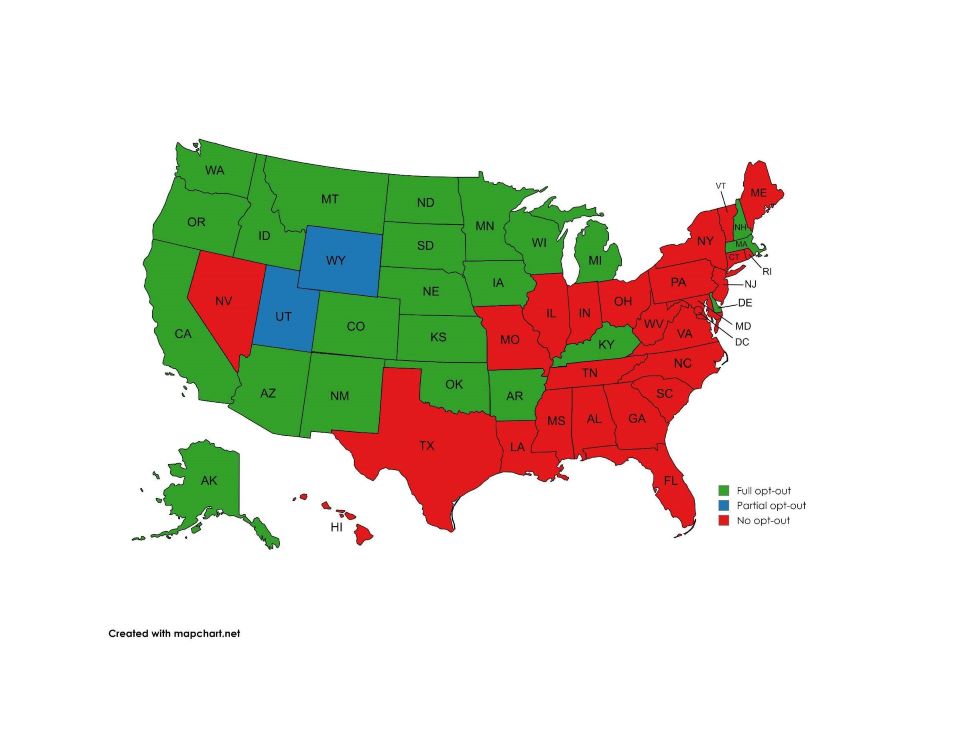
The map below identifies the states that have so far chosen to opt-out of the requirement, with more working to make this change each year.
States that have opted out have increased access to safe, affordable anesthesia care by removing barriers and allowing healthcare facilities to maximize their workforces. These decisions recognize that CRNAs are qualified to make decisions regarding all aspects of anesthesia care based on education, licensure, and certification.
Nationally, CRNAs safely administer more than 50 million anesthetics to patients each year working in every setting in which anesthesia is delivered. CRNAs are the primary providers of anesthesia care in rural settings, enabling facilities in these medically underserved areas to offer obstetrical, surgical, pain management, and trauma stabilization services. CRNAs have full practice authority in the Army, Navy, and Air Force and are the predominant provider of anesthesia on forward surgical teams and in combat support hospitals.
This process can be arduous and requires advocacy of CRNAs like you. If you’d like to get more involved in advocating for Virginia to become an opt-out state, reach out to Cathy Harrison at [email protected]