VANA Opposes SB 882 & HB 1647: Bills Will NOT Solve the Anesthesia Workforce Problem in Virginia
Note: HB 1647 is expected to come before the House Health and Human Services Committee on Thursday, Jan. 30. SB 882 has been referred to the Senate Finance and Appropriations Committee and may come before the committee later this week. Please contact your lawmakers to tell them to vote no on these bills by clicking here.
Sen. Mamie Locke and Del. Cliff Hayes Jr. have introduced legislation, Senate Bill 882 and House Bill 1647, respectively, that would direct the Board of Medicine to establish criteria for licensing a brand-new category of anesthesia provider called “anesthesia assistant,” also known as Certified Anesthesiologist Assistants (CAAs).
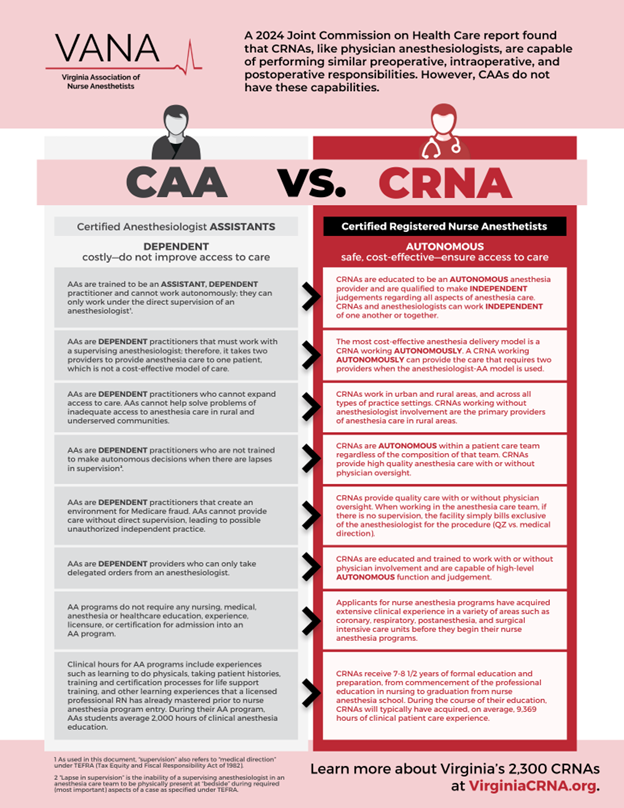
Unfortunately, licensing CAAs does nothing to improve the anesthesia workforce problem; CAAs drive up costs and make it harder to train anesthesia providers. CAAs must be directly supervised by a physician anesthesiologist, making CAAs one of the costliest anesthesia providers with no scientific evidence of increased patient safety.
Even more, a 2017 report from the Virginia Department of Health Professions found that CAAs reduce the number of clinical rotations available for anesthesia care providers and recommended against licensing CAAs in Virginia. Licensing CAAs will have an immediate negative impact, reducing the already limited training clinical rotation opportunities for Virginia’s 400 CRNA students across the state.
In late 2024, a report from the Joint Commission on Health Care recommended studying the impact of bringing CAAs to Virginia before considering immediately licensing them.
CAAs are one of the costliest anesthesia providers with no scientific evidence of increased patient safety.
With a CAA, the need exists to educate and use two providers — the supervising physician anesthesiologist and the CAA — to provide anesthesia care to a single patient. According to the American Academy of Anesthesiologist Assistants (AAAA), CAAs are limited by their
training and licensure to provide clinical support to anesthesiologists and may not practice “apart from the supervision of an anesthesiologist.” Because CAAs must be directly supervised by an anesthesiologist, the CAA/physician anesthesiologist team is one of the costliest anesthesia delivery models, and there is no scientific evidence of increased patient safety.
CAAs will not address the workforce shortage for anesthesia services in Virginia.
CAAs have a limited ability to meet patient anesthesia needs. There are approximately 3,500 CAAs in the U.S. versus over 65,000 Certified Registered Nurse Anesthetists (CRNAs). The fact that CAAs have not proliferated despite being in existence for approximately 60 years is evidence of their limited value. An estimated 3,000 new CRNAs enter the workforce annually, compared with about 300 new CAA graduates. Virginia has three CRNA training programs at Mary Baldwin University, Old Dominion University, and Virginia Commonwealth University, while there are no CAA training programs in Virginia. The number of new CRNAs entering the workforce yearly is about the same as the number of CAAs practicing nationwide. Given the cost-effectiveness of utilizing CRNAs on the anesthesia care team, expanding CRNA opportunities in Virginia makes more sense before licensing less experienced and more expensive CAAs.
CAAs hinder opportunities for expanding anesthesia care services.
Given that CAAs can only practice under the supervision of a physician anesthesiologist due to their limited education and training, their geographical reach is restricted to facilities where physician anesthesiologists practice. The vast majority of Virginia’s nearly 1,200
physician anesthesiologists practice in high population areas, leaving rural communities underserved. ODU and VCU Nurse Anesthesia Program Directors state licensing CAAs will have an immediate negative impact affecting the clinical rotation spots available to train CRNAs.
It is virtually impossible to assess the quality and safety of CAAs.
CAAs are limited by their training and licensure to provide clinical support to physician anesthesiologists and may not practice without direct physician anesthesiologist supervision. Because of this, it is nearly impossible to assess the quality and safety of CAAs because they cannot work apart from physician anesthesiologists. CAAs are not required to have any prior healthcare education or experience before they begin their CAA educational programs. Unlike CRNAs, CAAs have not learned to assess and treat a broad range of health problems before beginning anesthesia training. All these factors contribute to an anesthesia provider’s safety, and CAAs do not measure up against the proven safety of CRNAs.
Stand with CRNAs and OPPOSE SB 882 & HB 1647. Learn more about Virginia’s 2,300 CRNAs at VirginiaCRNA.org.